Accelerate Pheno® system
Actionable phenotypic susceptibility results obtained directly from a positive blood culture in approximately 7 hours to quickly initiate appropriate antimicrobial therapy1,2
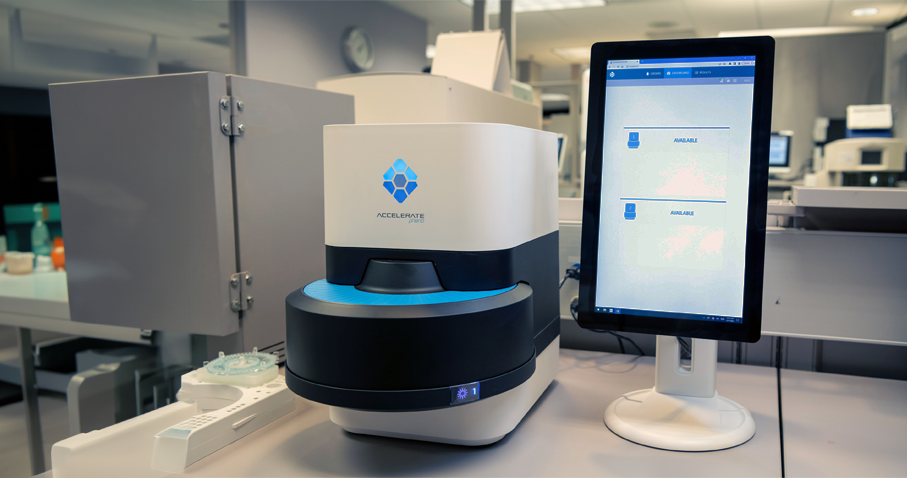

The Accelerate Pheno® system is designed to help clinicians expedite antimicrobial therapy decisions by providing fast, actionable phenotypic susceptibility results.2

80% of septic shock patients can be saved when appropriate antibiotic therapy is started within the first hour following onset of hypotension3
Delayed or inappropriate initial antimicrobial therapy for bloodstream infections results in prolonged hospital stays and increased mortality rates, while contributing to the silent pandemic of antimicrobial resistance.4-6
Healthcare institutions need rapid diagnostic instruments, including fast phenotypic platforms that facilitate earlier initiation of optimal therapy, to support their antimicrobial stewardship efforts and improve patient outcomes.2,7-9
Fast, fully-automated actionable results
The fully automated Accelerate Pheno® system provides microorganism identification in approximately 2 hours and minimum inhibitory concentration (MIC)-based susceptibility results in approximately 7 hours total, directly from positive blood culture.1,2
The fast phenotypic susceptibility results obtained with the Accelerate Pheno® system have been clinically demonstrated to help clinicians reduce time to optimal antimicrobial therapy and improve hospital length of stay.2,8-10
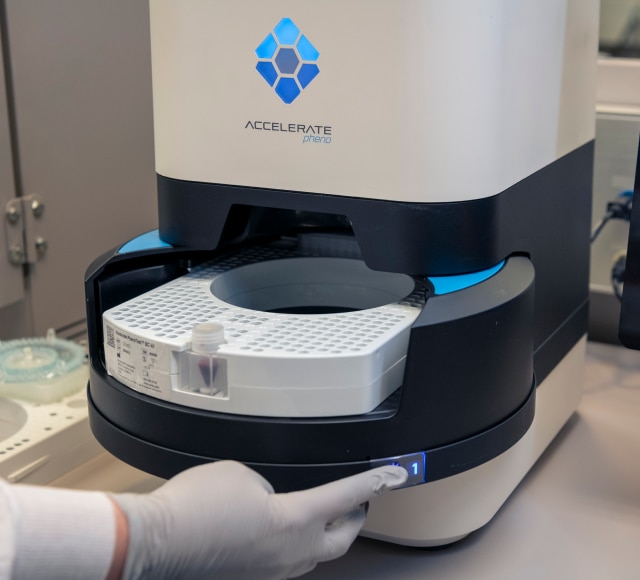
In addition, the Accelerate PhenoTest® BC kit is simple to use and easy to integrate into the laboratory and only requires 2 minutes of hands-on time per sample.11

Complementary solutions for your identification and antimicrobial susceptibility testing needs
The BD Bloodstream Infection Solution allows you to obtain complementary identification and antimicrobial susceptibility testing results that cover many of the microbiological needs of infectious disease specialists:
- Ensure rapid and robust pathogen identification with the BD™ Bruker MALDI Biotyper® System.12-14
- Detect known and emerging antimicrobial resistance using the comprehensive panel format of the BD Phoenix™ M50.15,16
- Leverage the speed of the Accelerate Pheno® system to provide fast, actionable phenotypic susceptibility results earlier to clinicians for critical specimens.1,2
Antimicrobial stewardship programs, combined with rapid diagnostics, are critical to optimize the use of antibiotics, effectively treat infections, protect patients from harm caused by unnecessary antibiotic use, reduce the risk of developing antibiotic resistance and reduce hospital costs and length of stay.2,4-9
Compared to conventional methods, the Accelerate PhenoTest® BC kit used in conjunction with antimicrobial stewardship efforts allow you to:
-
Get results faster
Time to antimicrobial susceptibility results accelerated by up to 40 hours17,18
-
Treat patients sooner
Time to optimal antibiotic therapy reduced by over a day9,10,19
-
Free up hospital beds
Length of stay shortened by up to 1.8 days8-10
Complementary ID/AST solutions for fast, actionable identification and susceptibility results

Bloodstream Infection

Magnolia Medical Technologies

Accelerate Diagnostics
*By clicking this link you are leaving bd.com and going to a third party website. Steripath® is a registered trademark of Magnolia Medical Technologies. Pheno® is a registered trademark of Accelerate Diagnostics.
- Accelerate PhenoTest® BC kit Instructions for Use (LBL000607).
- Bhalodi AA et al. Clin Infect Dis. 2022;75(2):269–77.
- Kumar A et al. Crit Care Med. 2006;34(6):1589–96.
- Battle SE et al. J Antimicrob Chemother. 2017;72(1):299–304.
- Burnham J et al. Open Forum Infect Dis. 2017 Oct 4;4(Suppl 1):S623–4.
- Bauer KA et al. Open Forum Infect Dis. 2022;9(11):ofac537.
- Mohayya SM et al. Antimicrob Steward Healthc Epidemiol. 2023;3(1):e22.
- Sheth S et al. Antimicrob Agents Chemother. 2020;64(9):e00578–20.
- Walsh TL et al. Infection. 2021;49(3):511–9.
- Dare RK et al. Clin Infect Dis. 2021;73(11):e4616–26.
- Sze DTT et al. BMC Microbiol. 2021;21(1):350.
- BD™ Bruker MALDI Biotyper CA System User Manual (8603291).
- Saffert RT et al. J Clin Microbiol. 2011;49(3):887–92.
- Knabl L et al. Lett Appl Microbiol. 2021;73(1):2–8.
- BD Phoenix™ M50 Automated Microbiology System User's Manual (500008930).
- Carey RB et al. Failure of Automated Systems to Detect Vancomycin-Resistant Staphylococcus aureus. Abstract presented at the Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC), Washington, DC, 2004.
- Charnot-Katsikas A et al. J Clin Microbiol. 2018;56(1):e01166–17.
- Marschal M et al. J Clin Microbiol. 2017;55(7):2116–26.
- Lutgring JD et al. J Clin Microbiol. 2018;56(4):e01672-17.
- Watanabe N et al. J Infect Chemother. 2022;28(4):563–8.
- Tenover FC et al. Emerg Infect Dis. 2006;12(8):1209–13.
- Kulah C et al. BMC Infect Dis. 2009;9:30.
- Mittman SA et al. J Clin Microbiol. 2009;47(11):3557–61.
- Woodford N et al. J Clin Microbiol. 2010;48(8):2999–3002.
- Hotaling M. Jt Comm J Qual Patient Saf. 2009;35(2):100–61.
- Mouser A et al. J Appl Lab Med. 2017;2(2):201–10.
- Merrill VD et al. J Appl Lab Med. 2022;7(2):532–40.
- Padoan A et al. Clin Chim Acta. 2020;500:213–9.
- Bell M et al. J Emerg Nurs. 2018;44(6):570–5.
- Arenas M et al. J Emerg Nurs. 2021;47(2):256–64.
- Zimmerman FS et al. Am J Infect Control. 2019;47(7):822–6.
- Nielsen LE et al. J Hosp Infect. 2021;120:127–33.
- Povroznik MD. Am J Med Qual. 2022;37(5):405–12.