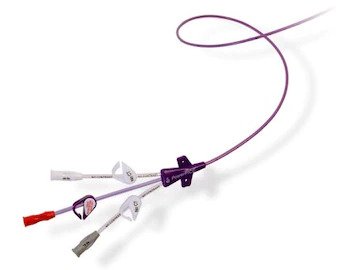
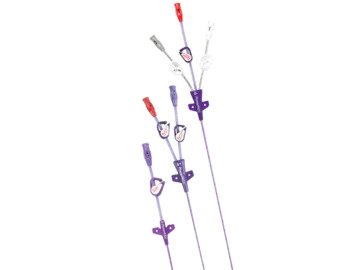
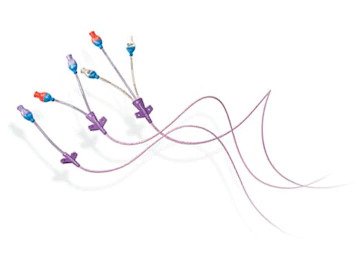
BD Peripherally Inserted Central Catheters (PICCs)
Optimizing vascular access management at each step

- Overview
- BD Solutions
A common device,
Vascular access devices (VADs) are used in virtually all pre-hospital, medical, surgical, critical care specialties, home-care settings and long-term care for infusion therapy, blood sampling and monitoring.1,2
Billions of VADs are placed worldwide annually3 with up to 90% of all hospitalized patients undergoing IV therapy,4-6 resulting in substantial healthcare expenditures.4
Even under ideal clinical conditions, nosocomial infections, such ascentral line-associated bloodstream infections (CLABSIs), are especially concerning given the plethora of associated comorbidities, including thrombosis,7 phlebitis8 and bacteremia.7
Billions of VADs placed annually worldwide3
Up to 90% of all hospitalized patients undergo IV therapy4-6
Nosocomial infections (e.g., CLABSIs) are especially concerning given associated comorbidities, including thrombosis,7 phlebitis8 and bacteremia7
Patients deserve an optimized, expert approach
Given the potential clinical and financial benefits of optimized vascular access (VA) practice, there is an imperative to establish VA teams (VATs) with expertise in VAD selection, placement and management.9,10
Vascular access management is the comprehensive category of products, solutions and services providing a continuum of vascular access care, from patient assessment to device removal, designed to reduce vascular access related complications.11
VATs are a strongly recommended approach
Specialized training in VA may reduce VAD failure rates, leading to better clinical and economic outcomes. Multiple observational studies demonstrated improvements in various clinical, efficiency and patient-reported outcomes associated with dedicated VA personnel.12-21
In the 2024 Standards of Practice, the Infusion Nurses Society22 states that VATs provide "proactive assessment of patient needs and selection of the most appropriate VAD, using evidence-based insertion techniques" and can help:
- Reduce the need to escalate more invasive devices
- Reduce costs associated with complications, labor and resources
- Positively impact patient satisfaction with improved first-attempt insertion success and fewer complications
In addition, the Centers for Disease Control and Prevention (CDC) and multiple published research demonstrate that the use of vascular access teams in the healthcare setting reduces mistakes and enhances patient safety, thereby indicating that the use of an infusion team is strongly recommended for all healthcare organizations.23
The value of building or optimizing a VAT
Shifting vascular access procedures from the interventional radiology (IR) suite to the bedside can create both clinical benefits and cost savings. Contact your local BD Vascular Access sales representative to learn more about data-driven tools to help determine the value of shifting procedure sites and how to build or optimize your current VAT.
-

Understand potential cost savings of shifting PICC catheter insertions from the IR suite to the bedside
-

Identify the number of FTEs needed to create or enhance a VAT based on responsibilities and clinical procedures
Optimizing vascular access management requires safe and effective solutions. Get to know the BD portfolio of category-leading peripherally inserted central catheters (PICCs), designed to support VAM optimization efforts and help reduce catheter-related complications.




- Carr PJ, Higgins NS, Cooke ML, Mihala G, Rickard CM. Vascular access specialist teams for device insertion and prevention of failure. Cochrane Database Syst Rev. 2018;3:CD011429.
- Carr PJ, Rippey JC, Cooke ML, Bharat C, Murray K, Higgins NS, et al. Development of a clinical predition rule to improve peripheral intravenous cannulae first attempt success in the emergency department and reduce post insertion failure rates: the Vascular Access Decisions in the Emergency Room (VADER) study protocol. BMJ Open. 2016;6(2):e009196
- Rickard CM, Marsh NM, Webster J, Gavin NC, McGrail MR, Larsen E, et al. Intravascular device administration sets: replacement after standard versus prolonged use in hospitalised patients-a study protocol for a randomised controlled trial (The RSVP Trial). BMJ Open. 2015;5(2):e007257.
- Dychter SS, Gold DA, Carson D, Haller M. Intravenous therapy: a review of complications and economic considerations of peripheral access. J Infus Nurs. 2012;35(2):84-91.
- Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but Unacceptable: Peripheral IV Catheter Failure. J Infus Nurs. 2015;42(3):151-64.
- Morrow S, DeBoer E, Potter C, Gala S, Alsbrooks K. Vascular Access Teams: A Global Outlook on Challenges, Benefits, Opportunities, and Future Perspectives. JAVA. 2022;27(1).
- Wilson Dib R, Chaftari AM, Hachem RY, Yuan Y, Dandachi D, Raad II. Catheter-Related Staphylococcus aureus Bacteremia and Septic Thrombosis: The Role of Anticoagulation Therapy and Duration of Intravenous Antibiotic Therapy. Open Forum Infect Dis. 2018 Oct 1;5(10):ofy249. doi: 10.1093/ofid/ofy249. PMID: 30377625; PMCID: PMC6201151.
- Haddadin Y, Annamaraju P, Regunath H. Central Line-Associated Blood Stream Infections. [Updated 2022 Nov 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430891
- Moureau NL, Carr PJ. Vessel health and preservation: a model and clinical pathway for using vascular access devices. Br J Nurs.2018; 27:(8)S28-S35. https://doi.org/10.12968/bjon.2018.27.8.S28
- Moureau N Establishing vascular access teams for patient safety. Infection Control Today. 2020; 24:(4)30-33
- https://www.bd.com/en-us/products-and-solutions/solutions/vascular-access-management
- Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle--journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care. 2013;17(2):R41.
- Savage TJ, Lynch AD, Oddera SE. Implementation of a Vascular Access Team to Reduce Central Line Usage and Prevent Central Line-Associated Bloodstream Infections. J Infus Nurs. 2019;42(4):193-6.
- Walker G, Todd A. Nurse-led PICC insertion: is it cost effective? Br J Nurs. 2013;22(19):S9-15.
- Reed SM, Brock AJ, Anderson TJ. CE: Champions for central line care. Am J Nurs. 2014;114(9):40-8; test 9.
- Johnson D, Synder T, Strader D. Positive Influence of a Dedicated Vascular Access Team in an Acute Care Hospital. JAVA. 2017;22(1):35-7.
- Cechinel R, Magalhães A, Nunes D. A dedicated vascular access and infusion therapy team in an acute care hospital: The benefits of reducing central line-associated bloodstream infections. J Vasc Access. 2018;20.
- Cais D, Armani J, Cardoso C. Is it worth having a dedicated infusion therapy nurse? Impact on peripherally inserted central venous catheter-associated bloodstream infections rates and costs. The 5th WoCoVA; Jun 19-212018.
- Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16:64.
- Zarbiv S, Manasia A, Griffiths S, Maddireddy P, Bamajboor M, Freeman R, et al. Extended-dwell peripheral intravenous catheters: A novel approach to decreasing central venous catheter utilization. Adv Neonatal Care. 2018;18(4):295-301.
- Shieh L, Go M, Gessner D, Chen JH, Hopkins J, Maggio P. Improving and sustaining a reduction in iatrogenic pneumothorax through a multifaceted quality-improvement approach. J Hosp Med. 2015;10(9):599-607.
- Nickel B, Gorski L, Kleidon T, et al. Infusion Therapy Standards of Practice, 9th Edition. J Infus Nurs. 2024;47 (1S Suppl1):S25-S26. doi:10.1097/NAN.0000000000000532
- Hadaway, L., Dalton, L., & Mercanti-Erieg, L. (2013). Infusion teams in acute care hospitals: A call for a business approach: An Infusion Nurses Society white paper. Journal of Infusion Nursing, 36(5), 356-360. doi:10.1097/NAN.0b013e3182a123a9.
BD-115725 (03/24)
A comprehensive approach to vascular access management
BD has a comprehensive category of products, solutions and services providing a continuum of vascular access care, from patient assessment to device removal, designed to reduce vascular access related complications.
Supporting your optimization efforts
As you strive to optimize your vascular access management practices, BD is here to support your efforts with proprietary assessments, tools and education.
-
Vascular Access Management assessments
BD assessments are unlike any in the industry. Using a proven methodology developed through years of experience and rigorous practice, each assessment is conducted by a clinically trained professional supported by proprietary, digital tools. The deliverable is a report filled with actionable data—analytics and benchmarks providing a clear road map with BD product recommendations and training to help you achieve improved clinical practices and outcomes.
-
Infusate Consideration Companion (ICC) tool and application
A critical step in reducing the risk of complications is to identify and recognize which medications and solutions may be associated with patient harm. The ICC may help you collaborate with an interprofessional team to identify medications that should and should not be given in peripheral veins.
-
Training resources
Our rigorous approach to vascular access education includes:
- A robust online learning platform with courses on PICC insertion, ultrasound, ECG placement, PICC placement and an FTE cost model
- Classroom training with bedside mentoring
- Access to a team of more than 75 clinical specialists dedicated to vascular access training and precepting